Examination of Peritoneal Fluid

The peritoneal cavity, a potential space within the abdomen, is lined with mesothelial cells and typically contains approximately 30-50 ml of serous fluid. This fluid, an ultrafiltrate of plasma, is formed through mechanisms involving hydrostatic pressure, plasma oncotic pressure, and capillary permeability.
When there is an abnormal accumulation of fluid in the peritoneal cavity, the condition is known as ascites, and the fluid is referred to as ascitic fluid.
Etiology of Ascites
The causes of ascites are detailed in Table 1, categorized based on whether the fluid is a transudate or an exudate. Unlike pleural fluid, there are no stringent criteria to distinguish between transudates and exudates in ascitic fluid. The majority of ascites cases are associated with liver cirrhosis, and the presence of ascites in cirrhotic patients indicates a poor prognosis.
| Transudate (increased hydrostatic pressure or plasma oncotic pressure) | Exudate (increased capillary permeability or lymphatic obstruction) |
|---|---|
|
|
Indications for Abdominal Paracentesis
Abdominal paracentesis involves the extraction of ascitic fluid by puncturing the peritoneal cavity. The indications for this procedure are summarized in Box 1.
Box 1: Indications for abdominal paracentesis
- All patients with new-onset ascites.
- At admission in all patients with ascites for detection of asymptomatic infection.
- All patients with ascites who develop clinical features of bacterial infection, hepatic encephalopathy, gastrointestinal hemorrhage, or impairment of renal function.
- Symptomatic ascites (therapeutic paracentesis).
Sample Collection
Ascites can generally be identified through clinical examination; however, when clinical findings are inconclusive, ultrasonography can be employed to confirm the presence and determine the cause of ascites.
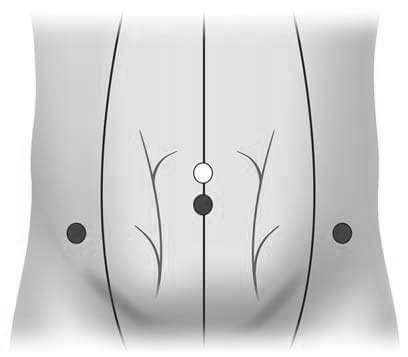
A hollow needle is inserted through the abdominal wall, typically in the left lower quadrant below the shifting dullness border, into the peritoneal cavity (Figure 1). Under aseptic conditions, 20-50 ml of fluid is extracted. For cytological analysis, 100 ml should be collected to enhance the yield of malignant cells. For cell count, the sample is collected in an EDTA-containing tube, and for microbiological culture, the sample is inoculated into blood culture bottles at the bedside.
Complications of abdominal paracentesis may include hemorrhage, perforation of the viscus, and infection. Contraindications include evidence of fibrinolysis or disseminated intravascular coagulation in liver disease.
Ascitic Fluid Analysis
Laboratory analysis of ascitic fluid aids in the differential diagnosis of ascites. The choice of tests should be tailored to the individual patient's clinical presentation. Commonly performed tests include total protein and albumin estimation, cell count, cytological examination, and bacterial culture.
Common Tests on Ascitic Fluid
- White Cell Count: This critical test quickly identifies potential bacterial infections. A neutrophil count greater than 250/cmm strongly suggests bacterial infection, while lymphocytosis indicates peritoneal tuberculosis or carcinomatosis.
- Albumin: Measuring serum and ascitic fluid albumin levels allows for the calculation of the serum-ascites albumin gradient (SAAG), which categorizes ascites into low and high SAAG.
- Microbiological Tests: These include Gram staining, Ziehl-Neelsen staining, and culture.
- Cytological Examination: This is used to detect malignant cells when cancer involves the peritoneum.
Appearance
Transudates are typically pale yellow or straw-colored and clear, whereas exudates tend to be opaque or turbid. Turbidity in the fluid can result from the presence of leukocytes, malignant cells, or proteins. Bloody or hemorrhagic fluid may indicate a traumatic tap, recent surgery, abdominal trauma, or malignancy. A traumatic tap is characterized by a gradual clearing of the fluid during aspiration. Milky or chylous fluid is often due to lymphatic duct obstruction caused by inflammation or malignancy (such as lymphoma or carcinomatosis), or by abdominal injury.
Chemical Examination
Proteins
Traditionally, a fluid is classified as a transudate if it has a low protein content and as an exudate if the protein content is high. However, this criterion alone is not always sufficient for reliable classification. In ascitic fluid, the differentiation between transudates and exudates cannot be dependably made based solely on protein estimation. A more accurate indicator is the serum-ascites albumin gradient (SAAG), which is calculated as the difference between serum albumin and ascitic fluid albumin measured on the same day (see Flowchart 1). The total protein concentration in ascitic fluid is useful for distinguishing spontaneous bacterial peritonitis (total protein <1.0 g/dl) from secondary bacterial peritonitis (total protein >1.0 g/dl).
- Serum to ascites albumin gradient (Serum albumin) — ascites albumin in gm/dl
- High albumin gradient (≥1.1) ascites
- Cirrhosis of liver
Congestive cardiac failure
Constrictive pericarditis
Budd-Chiari syndrome
Massive liver metastases
- Cirrhosis of liver
- Low albumin gradient (<1.1) ascites
- Tuberculous peritonitis
Peritoneal carcinomatosis
Biliary peritonitis
Pancreatic ascites
Nephrotic syndrome
Serositis
- Tuberculous peritonitis
- High albumin gradient (≥1.1) ascites
Lactate Dehydrogenase
The concentration of lactate dehydrogenase (LDH) in ascitic fluid is elevated in cases of spontaneous bacterial peritonitis (where there is no obvious source of infection), secondary bacterial peritonitis (where an identifiable source of infection is present), and peritoneal carcinomatosis. Table 2 outlines the ascitic fluid characteristics associated with various diseases. The differences between spontaneous and secondary bacterial peritonitis are detailed in Table 3 and depicted in Flowchart 2.
| Cause | Appearance | Type of fluid | Cells | Special studies |
|---|---|---|---|---|
| Spontaneous bacterial peritonitis | Cloudy or turbid | Exudate | Neutrophils ≥250/μl | Single organism isolated on culture; Proteins <1.0 gm/dl; Glucose normal |
| Secondary bacterial peritonitis | Cloudy or turbid | Exudate | Neutrophils ≥1000/μl | Multiple organisms isolated on culture |
| Cirrhosis of liver | Clear, straw-colored | Transudate | Lymphocytes <500/μl | Albumin gradient ≥1.1 gm/dl |
| Tuberculous peritonitis | Serosanguineous | Exudate | Lymphocytes >500/μl | Ziehl-Neelsen stain; culture; Low albumin gradient; Total proteins ≥2.5 gm/dl |
| Malignancy | Bloody | Exudate | Lymphocytes, malignant cells | Cytology |
| Parameter | Spontaneous bacterial peritonitis | Secondary bacterial peritonitis |
|---|---|---|
| Obvious source of infection | Absent | Present, e.g. perforation of viscus, abscess |
| Total ascitic fluid proteins | <1.0 gm/dl | ≥1.0 gm/dl |
| Severity | Less severe | More severe |
| Culture | Single organism | Multiple organisms |
| Treatment | Rapid response to antibiotics | Requires surgical treatment |
- Polymorphonuclear neutrophils in ascitic fluid ≥250/cmm
- Total proteins and glucose in ascitic fluid; culture of ascitic fluid
- Protein ≥1 gm/dl; low glucose; multiple organisms grown on cluture
- Secondary bacterial peritonitis
- Bile-stained fluid
- Biliary perforation
- Free air under diaphragm
- Intestinal perforation
- Bile-stained fluid
- Secondary bacterial peritonitis
- Protein <1 gm/dl; glucose normal; single organisms grown on cluture
- Spontaneous bacterial peritonitis
- Protein ≥1 gm/dl; low glucose; multiple organisms grown on cluture
- Total proteins and glucose in ascitic fluid; culture of ascitic fluid
Amylase
Typically, the level of amylase in ascitic fluid is comparable to that in serum. However, if the ascitic fluid amylase is more than three times the serum amylase level, it strongly suggests that the ascites is due to pancreatic disease, such as acute pancreatitis.
Bilirubin
An ascitic fluid bilirubin level exceeding 6.0 mg/dl and a ratio of ascitic fluid bilirubin to serum bilirubin greater than 1.0 are indicative of biliary tract perforation, also known as biliary peritonitis. In such cases, the ascitic fluid is bile-stained.
Cell Count
Cell counts are typically performed to differentiate cirrhotic ascites from spontaneous bacterial peritonitis. A total leukocyte count greater than 500/ml and an absolute neutrophil count exceeding 250/ml in the ascitic fluid are strong indicators of spontaneous bacterial peritonitis.
Microbiological Examination
A Gram stain is positive in approximately 25% of spontaneous bacterial peritonitis cases. If ascitic fluid is inoculated into blood culture bottles at the bedside, the sensitivity of pathogen isolation increases to 85%, compared to the conventional method of inoculating broth and agar plates in the laboratory. In spontaneous bacterial peritonitis, typically a single organism is isolated, whereas secondary bacterial peritonitis tends to be polymicrobial. For tuberculosis, the Ziehl-Neelsen stain has a sensitivity of 25-30%, while culture yields positive results in about 50% of cases. A laparoscopic biopsy is often more useful for diagnosing tuberculous peritonitis.
Cytological Examination
Cytological analysis of peritoneal fluid can detect malignancy in 40-65% of cases of malignant ascites.
References
- Thomsen TW, Shaffer RW, White B, Setnik GS. Paracentesis. N Engl J Med 2006;355: e21.
- Thomsen TW, DeLaPena J, Setnik GS. Thoracentesis. N Engl J Med 2006;355:e16.
- Comment
- Posted by Dayyal Dg.
- Exudate
- Dialisis Peritoneal
- Transudate and Exudate
- How Does Dialysis Work
- Ascites Cirrhosis
- What is Peritoneal Dialysis
- Microscopic Examination of Peritoneal Fluid
- Chemical Examination of Peritoneal Fluid
- Physical Examination of Peritoneal Fluid
- Explain the Collection and Examination of Peritoneal Fluid
- Peritoneal Fluid Analysis
- Peritoneal Fluid Cytology
- Peritoneal Fluid Removal
- Peritoneal Fluid Cell Count
- Peritoneal Fluid Infection
- Peritoneal Fluid Cancer
- Peritoneal Fluid Definition
- Peritoneal Fluid Amylase
- Peritoneal Fluid Albumin
- Peritoneal Fluid Differential Count
- Peritoneal Fluid After Hysterectomy
- Peritoneal Fluid Gram Stain
- Pathology
- Pathology Notes
- Clinical Pathology